Endoscopic Sleeve Gastroplasty and Quality of Life: An In-depth Analysis Based on the Latest Data
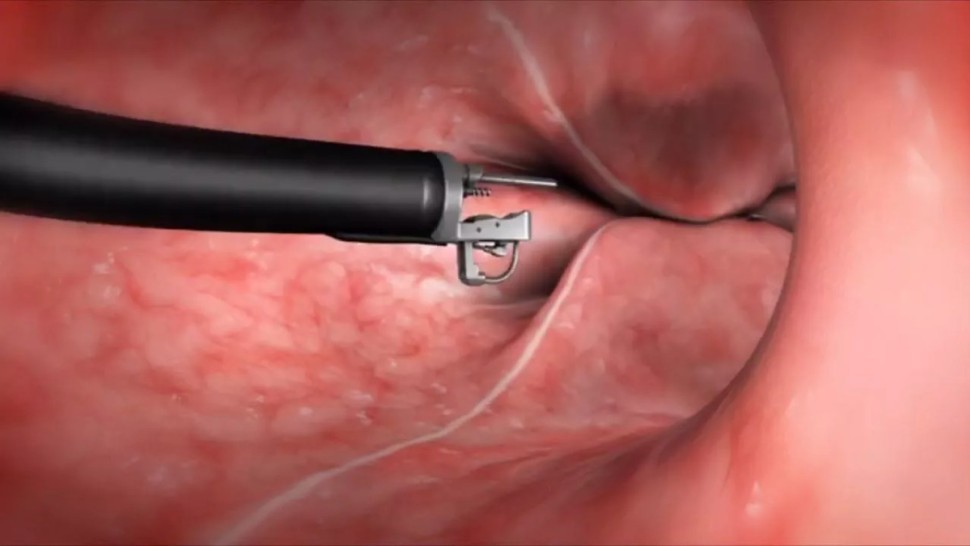
Endoscopic sleeve gastroplasty, also known as gastric endoscopic gastroplasty, is a minimally invasive, incision-free procedure that offers several advantages over other bariatric surgery techniques [1].
This procedure is becoming increasingly popular due to its simplicity and encouraging results in terms of weight loss and improved quality of life [2].
This article examines the latest data on endoscopic sleeve gastroplasty and its impact on patients' quality of life, based on an in-depth review of the scientific literature.